Pathological disorder of the peripheral nerves is Parsonage- Turners syndrome (PTS), also called neuralgic amyotrophy or shoulder neuritis. PTS generally occurs with an episode of severe shoulder pain, which lasts from a few days to weeks, following severe atrophy and weakness in one or more shoulder and shoulder muscles. Here we are going to discuss the parsonage turner syndrome. So, let’s start.
Parsons-Turner Syndrome (PTS):
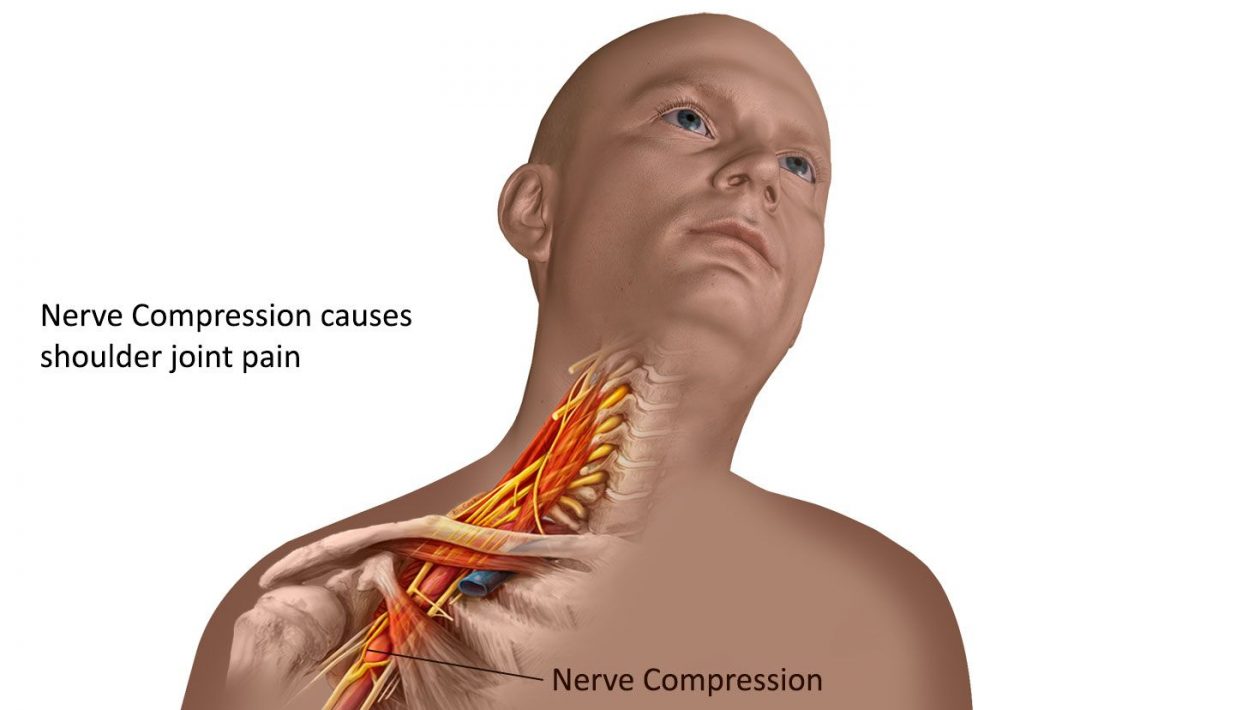
Parsons-Turner Syndrome is an uncommon neurological condition that develops rapidly in the shoulders and arms of extreme pain. In this actual process, muscle wastage and fatigue (amyotrophy) were found in the affected areas from several hours to weeks. PTS consists of a brachial plexus that extends from the spine to the neck and from any armpit and back. The nervous system controls movement and sensation in the shoulders, arms, and elbows. There might be other nerves in the arm or leg.
The precise cause of the PTSD is not clear, although an abnormality (immune-mediated disorder) in the immune system is supposed to prevent it. The seriousness of the injuries, particularly the actual nerves involved, can differ from person to person. Persons affected can recover without treatment, and so the strength returns to the muscles concerned, and the pain disappears. Even so, prolonged periods can occur. Residual and severe disabilities can exist in some people.
PTS Symptoms:
Sudden onset of discomfort (unilateral pain) in one shoulder is a signature feature of PTS. In some situations, the starting point may be sudden, and in others, the initiation of pain may be slow and gradual. Dain within the same edge of the shoulder may impact the neck, arms, and hand.
Again, it should be remembered that parsonage turner syndrome is a complex condition that may not represent any person’s situation. Some people (roughly 75%) had one episode only, while others (approximately 25%) experienced events repeatedly. Repeated symptoms may include a variety of joint and separate peripheral nerves; the peripheral nerves directly affected. The intensity, duration, and pain location vary between individuals.
In the evening or at night, the suffering is often steady and extreme.
The pain may be intense and slow. The acute process can be called this initial stage. The person afflicted is incremental, with little discomfort (i.e., rest) whether the injured shoulder or arm is not utilized. The pain increases gradually with time.
Therefore, basic movements can cause the condition worse and may take hours before intense and severe pain occurs. This occurs due to the abnormally sensitive (hypersensitive) initially damaged nerves. Progressively, the patient develops chronic, low-grade anxiety, sometimes known as a continuous period, lasting for one year or more.
The severity of muscle deficiency can differ tremendously from mild to uncommon muscle paralysis. People with PTS triggered muscle fatigue and nerve trauma to the muscles of the shoulders and arms.
The extent of the weakness depends on the number of nerves.
Besides fatigue, the impact muscles become increasingly compressed and weaker (atrophy).
The deep, unpleasant, or uncomfortable feeling of the skin in the places under strain (hypothesis), tightness, discomfort (esthesia), or illumination (dysplasia) in the region under threat. (dysplasia).
In some cases, there may be additional complications.
Due to the exhaustion and weakening of the muscles concerned, the hands, back, braces and limbs will significantly alter. In this case, the affected individual is in danger of secondary intrusion or conjecture. Secondary impetrations are a severe disorder in which the shoulder muscles compress or widen as the arm travels.
Individuals afflicted are more prone to cause contracture, which contributes to irregular muscle- and tendon-contraction, deformity, or rigidity of the joint. The arm’s contraction, also known as adhesive capsulitis, will trigger discomfort and reduce the usual articular range.
Often the lumbosacral plexus nerve may include nerves beyond the brachial plexus, such as the antifungal nerve or the chronic laryngeal nerve. Lower spinal nerves (lumbosacral plexus) can trigger discomfort, hypoesthesia, and leg paranesthesia. Organ transmits impulses to the cortex, the organ that divides the lungs from the abdomen. Antifungal nerve intervention may cause significant breathability. Recurrent involvement of laryngeal nerves may lead to vocal cord weakness and partial paralysis resulting in the rough and mild talk (pituitary). Most seldom, the face or other scalp can be affected.
The nerve injury to the PTS will impact the arteries of blood and cause more signs, mainly on the hands, including redness, bruises, and spots on the skin. Fluid retention (edema) may cause inflammation. Body, hair, and nails are rising quicker than ever before. Some parts of the body, particularly the hands and wrists, cannot respond correctly to outside temperatures. Extreme suddenness may occur, or excessive cold can occur in the impacted areas.
Some people may recover the complete shoulder or region intensity and functional status.
Several medical literature studies suggest that in two years, most people should regain up to 70% to 90% of their original capacity. Recent findings have shown that some patients require longer than two years, and some suffer symptoms, including persistent, recurrent discomfort, arm motions, and knee disorders. Severe disabilities can impair your capacity to function and routine tasks in critical circumstances.
Reasons for PTS:
It is not entirely known the exact cause of the TCP. In some instances, researchers believe that there is an inflammatory immune-mediated reaction to certain infections or predisposing factors that destroy the brachial plexus nerves. The most critical risk factor in the progression of the condition is the latest viral illness. Birth may cause PTS in women. In some cases, it is impossible to identify the triggering event or underlying factors.
Some scientists believe that specific individuals will grow PTS as a consequence of the exposure mentioned above.
PTS has a higher impact on men than on females.
This disease has been measured at roughly 1.64-3.00 persons per 100,000 individuals in the adult population and based on current longitudinal surveys. However, cases with PTS can be misdiagnosed or misdiagnosed, such that the actual prevalence in the community may be considered challenging. In teenagers and middle-aged people, the situation most often begins to develop, but young children and women have also been identified.
Some certain diseases or illnesses may induce signs of PTSD. Disorder, chronic degenerative inflammatory eligibility, polymyalgia, chest salad disorder, and brachial plexus (brachial neoplastic plexus) affect. For other factors, glutinous capsulitis, which can grow as a PTS complication. NORD focuses on these conditions and has a general peripheral neuropathy study. (Select a particular condition name in the rare disease spreadsheet as a search term for more relevant data.)
Diagnosis of PTS:
PTS diagnosis is based on characteristic indications, a detailed medical history, a thorough clinical assessment, and different particular tests. Specific tests can be used for assessing the condition of muscles and nerves that control muscles, including studies of neuro-conduction and electromyography.
The electrodes strengthen the nerves and monitor the conductivity of the signal. The electrode records the dynamic behavior of the muscle fibers. This entry illustrates how the muscle reacts to the nervous system and whether these muscles are weakening the flesh or the nerves controlling them.
To achieve transverse images of particular organs and body cells, MRI uses a magnetic field, and radio wave MRI may help eliminate certain potential factors, such as physical tiredness, shoulder pain, and signal adjustments triggered by nervous system absence.
Treatment of PTS:
Therapy leads to some symptoms, which occur in every individual.Orthopedics, neurologists, neuromuscular disease specialists, pediatricians, practitioners, and other medical practitioners must systematically and comprehensively plan for an individual’ s treatment. To increase the chances of full recovery, early intervention, and precise treatment are essential.
In certain situations, PTS may include self-treatment and support services only, for example, specific pain relief approaches like pain medicine. Some doctors suggested using oral corticosteroids during the acute phase, such as prednisone, reducing pain length, and, in some instances, accelerating the treatment process. However, for many people, corticosteroids have proved useless and have harmful side effects. Only sure doctors do not, therefore, suggest their consumption.
Specific medications
Such drugs manage nerve pain directly. The diagnosis of patients with parsonage turner syndrome is achieved by exercise and functional exercises to retain muscle control and mobility of the joint affected.
Exercises that stimulate muscles during the acute period cannot be utilized in most situations because discomfort is intensified. Many strategies for PTS treatment include Heat Stimulation, or Ice, or Percutaneous Stimulation of the Electrical Nerve, to better regulate the pain by modification or obstruction of the movement of nerves across the skin.
However, Surgery can be considered in people who are not positively responding to other invasive treatments. Nerve implantation or tendon transplantation can require surgical procedures. Nerve transplantation is the extraction process of a nerve tissue piece to repair a destroyed part of the body. Neural implantation is an extraction process.
Tendon movement activity and injury muscle control.
This procedure can be done later (usually after two years) if it is impossible to restore the nerve. In this phase, one part of the body eliminates a right tendon, and another substitutes an injured or diseased cord. Such operations restore shoulder and joint mobility and work.
Many patients only undergo one case, recovering their power and mobility entirely in the shoulder and other places impacted. According to old scientific literature, the bulk of people regain their initial intensity and work to as much as 70-90 percent. After its initial resolution or effective treatment, there is about a 5–26% risk of recurring PTS. For 10-20 % of cases, physical resistance or aversion to the damaged shoulder reduces constant discomfort.
For example, lifting or raising is difficult for others. Others can encounter problems with repetitive activities that damage their arm or shoulder. Some persons may have a winged scapula in which the scapula (scapula) rises behind or rises out from behind abnormally. People with chronic incidents are most likely to remain troublesome over a long period.
Conclusion:
in conclusion, Scientists are investigating the treatment of patients with parsonage turner syndrome using intravenous immunoglobulin. Also, If anyone has something to ask on this topic, please let us know in the comments below. if you have any queries about the parsonage turner syndrome please write you comment on below comment section. Thank you.